Describe the Soap Approach to Medical Record Documentation
SOAP or SOAP notes as they are widely called also find extensive usage in veterinary practices. SOAP Notes in the Medical Field.

Treatment Notes And Progress Notes Using A Modified Soap Format Musculoskeletal Key
The missing documentation included.

. Narrative notes in SOAP format are the clinical standard. Its imperative that every student learn the basics of writing a SOAP note to become a health care provider like a physician or an Advanced Practice Nurse. First record the risk-benefit analysis of important decisions in the clinical care of the patient.
The patients chart must reflect subjective findings that are consistent with a lesion injury or condition. SOAP notes were first developed by Dr. A SOAP note is just one of many documentation formats a therapist can use.
There are many styles of chart notes that can be effective. Written so it can be read Written in ink Written in clear language Written. More and more dental and medical insurance payers are demanding excellent clinical documentation in the form of SOAP format to back up procedures performed on patients that are members of their plans.
The O in SOAP denotes objective. SOAP finds its usage in recording patient progress. The term used to describe a patient who does not follow the medical advice given.
Be sure to record the patients temperature heart rate blood pressure respiratory rate and oxygen saturation. Definition of SOAP A method of documentation used by service providers to describe events that took place during time spent with individuals either on the phone or in person. Where a clients subjective experiences feelings or perspectives are recorded.
SOAP is an acronym for the 4 sections or headings that each progress note contains. An approach to medical records documentation that documents information in the following order. It is a way for clinics to record document and store patients medical.
A SOAP note is information about the patient which is written or presented in a specific order which includes certain components. The SOAP Acronym. However its also one of the oldest.
This risk-benefit analysis should include even obvious or given. The SOAP note is an essential method of documentation in the medical field. As a Certified Nurse-Midwife I use notes like these in everyday life.
Medicaid medical records should be legible. Lawrence Weed in the 1960s as part of the problem-oriented medical record POMR and quickly amassed widespread adoption as the primary method to document and distribute the problems identified by physicians. The key to this approach is to keep in mind the three sovereign principles of documentation which also closely resemble the three principles of medical decision analysis.
An EMR or EHR contains a wide variety of information like treatment history medical records patient progress etc. For now providers should understand that coders and auditors have an audit tool based on established documentation guidelines. Whether you are in the medical therapy counseling or coaching profession SOAP notes are an excellent way to document interactions with patients or clients.
SOAP notes provide a uniform and easy way of tracking a patients medical records. Whether covered by insurance or not good clinical notes support the rationale for treatment and are necessary should there be a lawsuit or medical issue that. Reviewing Records for Accuracy.
An approach to medical records documentation that documents information in the following order. SOAP notes are used for admission notes medical histories and other documents in a patients chart. Be sure that the medical terms are spelled accurately.
The S in SOAP denotes subjective which are noted down by the doctors or nurses for getting a reason for the patients visit. The Subjective Objective Assessment and Plan SOAP note is an acronym representing a widely used method of documentation for healthcare providers. In the second part of your day you will review medical documentation to ensure all information is accurate.
Start with the patients vital signs. The SOAP note is a way for healthcare workers to document in a structured and organized way. Plan of action symptom a subjective or internal condition felt by a patient such as pain headache nausea or other indication that generally cannot be seen or felt by the physician or measured by instruments.
This might include subjective information from a patients guardian or someone else involved in their care. Provide the effective pronunciation of the medical terms. Consistent documentation in line with your 19951997 based audit tool may help mitigate provider contention and encourage a team approach to health record audits and clinical documentation improvement programs.
Transition to your physical exam. They can also provide documentation of progress. Medical necessity documentation A Physician Certification Statement Required signatures.
Build medical terms by using the appropriate word parts. I am grateful that Ive gotten. Effective chart notes must reflect the four criteria required to document medical necessity.
SOAP notes are easy to use and designed to communicate the most relevant information about the individual. In this part the patients medical history is also noted down. At a minimum a medical record should be.
Up to 10 cash back The objective section of your SOAP note should unsurprisingly comprise objective information you collect from the patient encounter.
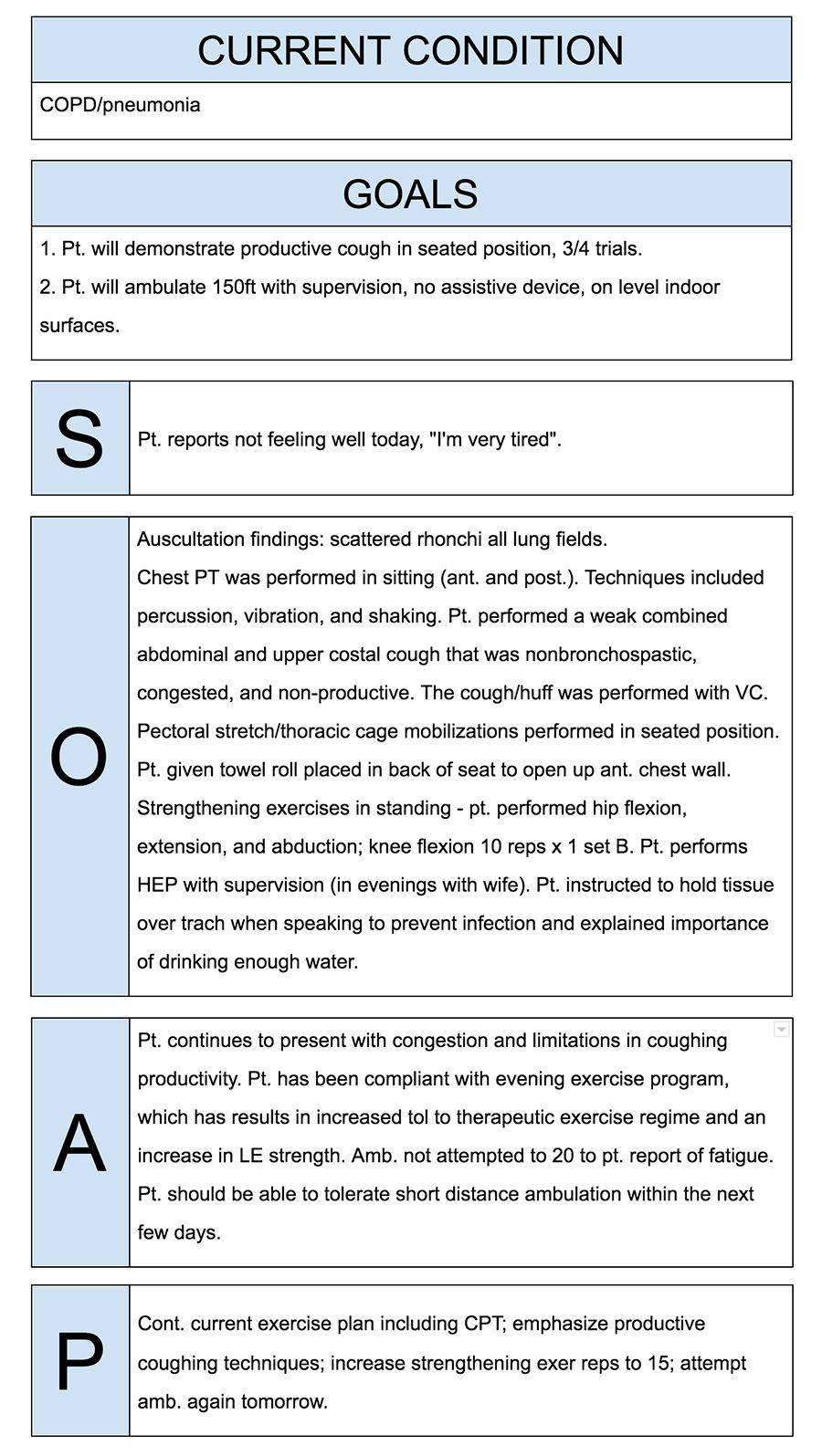
How To Write Incredible Physical Therapist Soap Notes

30 Soap Note Examples Blank Formats Writing Tips Soap Note Clinical Social Work Medical Terminology Study

The Evolution Of Office Notes And The Emr The Caps Note Consult Qd

46 Free Download Soap Note Template For Your Medical Note Soap Note Notes Template Doctors Note Template
Comments
Post a Comment